Parkinson's Disease has been celebrated worldwide on 11 April since 1997, through a joint initiative between the European Parkinson's Disease Association (EPDA) and the World Health Organization. The aim is to mark the date of birth of Dr James Parkinson, the English physician who first described this disease and pushed for its greater awareness.
Since April 2015, the disease has been represented by a red tulip and is used by various associations and organizations worldwide.
Interestingly, years earlier, in 1981, Dutch florist J.W.S. Van der Wereld, diagnosed with Parkinson's Disease, presented a red and white tulip that he had recently produced. He called it “Dr James Parkinson” to honour the doctor who characterized the illness.

This bright cardinal red tulip, with a white border on the petals and a whitish outer base, received some awards in several European countries.
Parkinson's disease, which is still incurable, affects body movements, causes tremors, stiffness, posture unsteadiness and changes in gait. It has been referred to since ancient times.
It is referred to as Kampavata (in Sanskrit "Kampa" means tremor) in Ayurveda, the oldest known Indian health system that has existed for over five thousand years ago. It started in the territory where India and Pakistan are now located.
Ancient Chinese documents refer to descriptions of Parkinson's disease. In Western medicine, doctor Galen describes this disease as "agitation paralysis".
In 1817, the text “An Essay on The Shaking Palsy”, by James Parkinson, was published. It was the first medical document to debate this disease.
James Parkinson was born on 11 April 1755 in Shoreditch, London, and died in the same city on 21 December 1824, victim of stroke.
Coming from an upper middle class family in London, his father John Parkinson, who was an apothecary and surgeon in Hoxton Square, was his great advisor and inspirer in his professional choice. Later, in 1794 with his death, James Parkinson inherited the apothecary, medical assistance and his work.
One of his concerns was the well-being and the living conditions of the population, especially those who suffered from mental illness.

While studying medicine at London Hospital Medical College, he also studied philosophy, Greek, Latin and shorthand. He obtained his diploma from the Royal College of Surgeons.
In 1777, James Parkinson was awarded the London Humanitarian Society medal for helping his father when they tried to resuscitate a man who had attempted suicide by hanging.
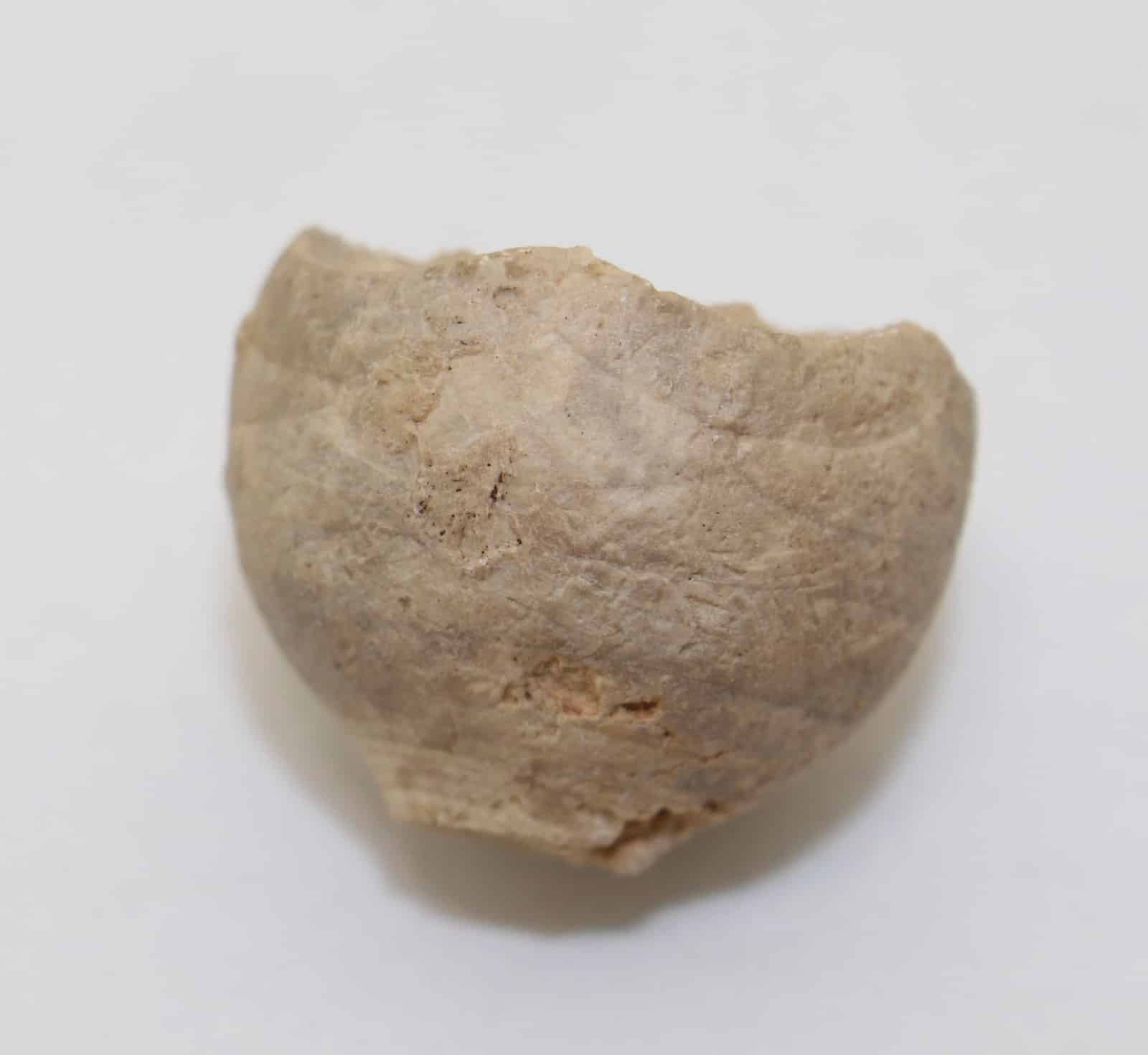
In addition to being interested in the medical field, geology and palaeontology (he was honoured by having his name given to some fossils such as Parkinsonia parkinsoni, a mollusc; Apiocrinus parkinsoni, a sea animal; Rostellaria parkinsoni, a snail, and Nipadites parkinsoni, a tree). In his early career years, James Parkinson was also involved in politics.

Always interceding on behalf of the least protected, he was a staunch critic of the government of Prime Minister William Pitter and an admirer of the ideals of the French Revolution. James Parkinson, under the pseudonym of Old Hubert, wrote and published more than two dozen pamphlets calling for profound changes both in society and in Britain's politics, defending the presence of the people in parliament and the universal vote.
As he became involved in secret political societies, he was suspected of having participated in a conspiracy to assassinate King George III, with the intention of causing a riot in order to shake up English society. However, the plan was not carried out because many of the rebels were arrested or exiled to the former British colony, Australia. James Parkinson was investigated, but he was spared.
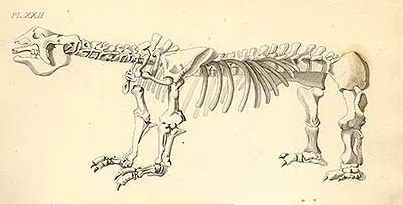
In 1804, he published the first volume of “Organic remnants of the ancient world”, where he exhibited, through his illustrations, fossils of animals and minerals. The second and third volume of this work sere published in 1811.

In 1805, he published the work “Observations on the nature of gout, on the nodules of the joints and on the influence of food on gout and rheumatism”.
In 1812, he was the first to identify the rupture of the vermiform appendix as a cause of peritonitis at the death of a five-year-old child, while working together with one of his sons, John, also a doctor. With this study, he sought to warn about the urgency of surgical treatment of this disease.
On 11 April 1817, James Parkinson published the scientific text entitled “An Essay on The Shaking Palsy”, where he described the symptoms of the disease (unsteadiness in posture and tremors in various parts of the body, mainly in the hands and arms) that affected six of his patients. This work was the first medical document to discuss this disease. From that time until today, the diagnostic criteria have changed little.

Years later, French physician Jean-Martin Charcot (1825-1893) proposed the name Parkinson's disease for shaking palsy.
Parkinson's disease is considered the second most common progressive neurodegenerative disease of the central nervous system in the world population, in addition to Alzheimer's disease.
It is thought that there are 10 million Parkinson's patients worldwide. In Portugal, it is estimated that 20 thousand Portuguese suffer from this disease and two thousand new cases of this pathology are identified every year.
According to the World Health Organization, about 1% of the world population aged 65 and older suffer from Parkinson's disease.

This disease, still incurable, chronic, of progressive evolution, which affects body movements, appears when the destruction of nerve cells occurs. Its pathology is still unknown, but it is believed that in addition to having genetic (3 to 4% of patients) and environmental causes, heredity (2 to 5%) and ageing (the highest percentage) are also considered risk factors, affecting individuals of both sexes, with a slight predominance in men.
Clinically speaking, Parkinson's disease occurs when neurons in a certain brain region (substantia nigra) die. Normally, these cells are responsible for the production of dopamine, which is a neurotransmitter that helps to transmit messages between the different areas of the brain that control body movements. When the cells of the substantia nigra die, there is a decrease in the levels of dopamine, which causes difficulty in controlling muscular and body movements. Muscles are affected both during rest and during activity.

In general, the first motor symptoms of this disease appear slowly from the age of 50 onwards (although they may appear as early as 30 or 40), and only years after the onset of the disease. So it is very difficult to diagnose it because it is only possible to discover it when tremors and slowness appear.
Researcher Hugo Vicente Miranda, from the Chronic Disease Research Centre at the Faculty of Medical Sciences of Universidade Nova de Lisboa, says that the disease starts “when loss of smell, constipation or depression occur. These symptoms precede the motor issues - when 60% of the population of dopamine neurotransmitters essential for the motor part of the brain to be activated and to allow the coordination of movements has already been lost.”

This disease has several manifestations, varying from individual to individual. The most common and early motor symptoms are hand and leg tremors and slow movement. As the disease progresses, the symptoms become more aggressive. The central nervous system is gradually adulterated, forcing the transmission of messages between nerve cells not to take place normally. Motor symptoms appear (muscle stiffness, gait difficulties, slowness and uncoordinated movements, lack of balance, tendency to fall, changes in body posture and facial expression), but non-motor signs (such as sleep disturbances, difficulty swallowing, loss of smell, depression, apathy, constipation, disturbances in urination, monotone voice, writing with increasingly smaller letters, and reduced reflexes) can also appear.
As there is no laboratory analysis to confirm this disease, the diagnosis of Parkinson's Disease is only possible by observing the patient's signs, symptoms, conditions, family history and neurological exams performed by the neurologist who may eventually screen out other curable neurological diseases that also affect body movements involuntarily.
Although Parkinson's disease has no cure, there are currently numerous therapeutic options that aim to control symptoms, delay the progression of the disease and improve the patients’ quality of life.
In addition to drugs (which must be used throughout the patient's life), whose function is to raise the insufficient levels of dopamine, there is also the possibility that patients are selected (according to the stages of the disease) to be subject to surgical interventions.
In addition to medication, it is essential that patients with Parkinson's disease have occupational therapy, physical exercises, physiotherapy, speech therapy, psychological and nutritional support. All these can increase their response capacity and adapt the body to the manifestations of the disease, in order to improve their daily activity, independence and have better quality of life. It is essential that the closest relatives obtain information and guidance so that they can support patients in the best possible way, to prevent them from becoming depressed, unmotivated and with low self-esteem.

Num artigo publicado no Jornal do Médico em 2015, investigadores do Instituto de Medicina Molecular (IMM) coordenados por Joaquim Ferreira, professor do Departamento de Neurologia e Farmacologia Clínica da Universidade de Lisboa, anunciavam que era possível detetar e diagnosticar a Doença de Parkinson (identificando a “Substantia nigra”) através da realização de uma ressonância magnética. Referiam que, esta identificação propicia direcionar a terapêutica "seleccionando um plano adequado para optimizar os recursos farmacológicos disponíveis e permitindo a definição do prognóstico, com marcadas implicações pessoais e familiares" e que “estes exames de imagem podem responder a dúvidas relativas ao diagnóstico da doença de Parkinson ou à sua diferenciação relativamente a outras situações clínicas.”
In an article published in Jornal do Médico, 2015, researchers from iMM, coordinated by Joaquim Ferreira, professor in the Department of Neurology and Clinical Pharmacology at the University of Lisbon, announced that it was possible to detect and diagnose Parkinson's Disease (identifying the “Substantia nigra”) by performing an MRI. They stated that, this identification allows to direct the therapy "selecting an adequate plan to optimize the available pharmacological resources and allowing the definition of the prognosis, with marked personal and family implications" and that "these imaging exams can answer questions regarding the diagnosis of the disease Parkinson's disease or its differentiation from other clinical situations.
Same year was published another article, in RTP-NOTICIAS, which referred to the phase III clinical trials of the drug Opicapone for Parkinson's Disease that Bial Laboratories developed and indicated a “significant decrease in the immobility period of patients, with the product being analyzed by the European Medicines Agency”.
At that time, Bial had already invested 200 million euros in the development of the medicine, with “the study involving 600 people from 106 centers”.
According to this study Joaquim Ferreira mentioned that "in the last 10 years there have been few options for new treatments for Parkinson's disease and Opicapone aims to respond to the need for a more potent COMT inhibitor". The data from this clinical trial were presented at the 12th International Congress on Alzheimer's and Parkinson's Diseases and related Neurological Disorders, which took place in Nice in 2015.
In recent years, several researchers, both national and foreign, have been looking at this pathology looking for new ways to control it.
We have, for example, a group of Portuguese researchers, including Hugo Vicente Miranda, Tiago Outeiro (from the Department of Experimental Neurodegeneration at the Medical Centre of the University of Göttingen, Germany) and Luísa Lopes (from the Institute of Molecular Medicine). They carried out a scientific study in 2018, funded by the Foundation for Science and Technology and supported by scientifically proven information in existence for sixty years. They found that there is a relationship between Diabetes and Parkinson's Disease. In that study, they report that “patients who develop type 2 diabetes between 25 and 45 years of age have a 400% chance of suffering from Parkinson's disease” and “a derivative of the sugar accumulated in the blood due to diabetes (glucose) can modify proteins, cause the death of neurons and lack of dopamine, which leads to the symptoms of Parkinson's disease”.
In an interview published in January 2021, neuroscientist Miguel Castelo-Branco (from the Institute for Biomedical Imaging and Translational Research, Faculty of Medicine, University of Coimbra) spoke about research (carried out by the Hospital and University Centre of Coimbra - CHUC, in collaboration with researchers from Coimbra - CIBIT and the Institute of Nuclear Sciences Applied to Health - ICNAS) aiming at “studying the brain's ability to readapt itself throughout life in health and disease” and create “a unique set of functional and molecular imaging methods that would allow eye movements to be assessed - a function that is altered very early in Parkinson's disease ”.

This study was published in the Proceedings of the National Academy of Sciences earlier this year, the first author being Diliana Rebelo, a CIBIT researcher. The study demonstrated that “the failure of the eye movement system is compensated in the early stages of the disease by increased recruitment of the part of the visual system that programmes it”. The authors found that “the functional compensation at the level of the structures that underlie communication between neurons: synapses” and the “levels of a type of dopamine receptor (D2), which is the key molecule in Parkinson's disease, adjusted in various parts of the brain, related to the programming of eye movements. This adjustment had an intimate relationship with the pattern of functional compensation found”, concluding that “there is a kind of reorientation of the eye circuits, of connection reforming, even at molecular level. It is almost as if there is a 'shift' to the most posterior part of the brain”. “The discovery of a link between synaptic plasticity and the reorganization of brain activity in Parkinson's disease opens the way for future work to understand the limits of the reorganization of the adult brain and its application to neurological rehabilitation” and “rehabilitation in patients with Parkinson's disease is possible. These results can have an impact on delaying the decline”
According to Miguel Castelo-Branco “this work also provides information on the effect of drugs, that is, it provides information that may be relevant for therapy, because dopamine is the central molecule in Parkinson's disease… When we look at the mechanisms of molecular compensation, we are left with much more information about the therapeutic effects of the drugs… namely, it gives clues to help prevent side effects associated with the therapy”.
Also in a study by researchers at the John Hopkins medical centre in the US and published in the American scientific journal Neuron in 2019, Ted Dawson, co-author and professor of neurology at Johns Hopkins University, demonstrated the inferences that Parkinson's Disease may start in the intestine.
This new study is based on work carried out in 2003 by the German neuroanatomist Heiko Braak (1937-) in which he demonstrated that “individuals with Parkinson's disease have defective alpha-synuclein concentrations in parts of the nervous system that control the gastrointestinal tract”. He believes that "the disease advances in the nerves connecting the gastrointestinal tract with the brain".
Since "Parkinson's disease is characterized by the accumulation of a defective protein, called alpha-synuclein, in brain cells, causing neural tissues to die, leaving behind large pieces of dead brain matter known as Lewy bodies. The death of brain cells is what affects a person's ability to move, think or regulate emotions”. Ted Dawson claims that the appearance of these proteins combines with some of the first signs of Parkinson's disease as the symptom of constipation.

After several experiments, Dawson concluded that, in general, “the defective alpha-synuclein protein can be transmitted from the stomach to the brain via the vagus nerve” and states that “this is an exciting discovery for the field and presents a target for early intervention in the disease”.
In the difficult times in which we live due to the Covid-19 pandemic, populations are more isolated, worsening the conditions of people, particularly those suffering from Parkinson's Disease. This is because they move less and may have atrophies, limited movement, loss of reflexes, and loss of communication and stimulation, which can increase depression and anxiety. Patients without family backing may also have less home support due to the scarcity of human resources that the pandemic has caused, changing their hygiene habits, food, treatment and access to medication.
In view of the conditioning factors of Parkinson's Disease, it is important to remember that we need to prevent these situations. Patients should try to keep the routines that were done before the pandemic, maintain the activities, have support in the domestic activities and assistance in the areas of food and hygiene.
Parkinson's patients should be encouraged to write, paint or perform simple activities, do physical exercises in accordance with the doctor's instructions, in the impossibility of going to physiotherapy and avoid being too long in front of the television. As it is a chronic disease, these patients need continuous medical evaluations, since the control of the disease is only achieved through regular medical monitoring. In the present situation, medical consultations can be carried out in person or via teleconsultation.
References:
Portuguese scientists make discovery related to Parkinson's disease. Available at: https://bomdia.eu/cientistas-portugueses-fazem-descoberta-relacionada-com-doenca-de-parkinson/. [Retrieved on 10-04-2021]
Another piece of the intricate relationship between diabetes and Parkinson's disease has been unveiled. Available at: https://www.publico.pt/2020/04/26/ciencia/noticia/desvendada-peca-relacao-intrincada-diabetes-doenca-parkinson-1913592. [Retrieved on 10-04-2021]
Study warns that the origin of Parkinson's disease is in the stomach. Available at: https://www.noticiasaominuto.com/lifestyle/1370074/estudo-alerta-que-origem-da-doenca-de-parkinson-esta-na-barriga. [Retrieved on 10-04-2021]
James Parkinson. Available at: https://www.wikiwand.com/en/James_Parkinson. [Retrieved on 10-04-2021]
Who was James Parkinson. Available at: https://hospitaldocoracao.com.br/novo/midias-e-artigos/artigos-nomes-da-medicina/quem-foi-james-parkinson/. [Retrieved on 10-04-2021]
Portuguese discover how to detect Parkinson's with blood test. Available at: https://iasaude.pt/index.php/informacao-documentacao/comunicacao-social/recortes-de-imprensa/4165-portugueses-descobrem-como-detetar-parkinson-com-analise-ao-sangue. [Retrieved on 10-04-2021]
World PD Day. Available at: https://www.parkinsonnet.lu/en/news-events/world-pd-day-2019. [Retrieved on 10-04-2021]
Lurdes Barata
Library and Information Area
Editorial Team

