Ovarian cancer is an uncommon disease, but has an unfortunately high mortality rate. This is largely due to nonspecific symptoms, which condition an often late diagnosis.
Its incidence is very variable worldwide, being the lowest in Africa and Asia and the highest in the countries of Eastern and Northern Europe. In Portugal, according to the latest published national cancer registry, the incidence is 6.2 per 100,000 women, corresponding to approximately 400 new cases of the disease each year. In the Western world, this number has increased in recent decades, understandable if we take into account that ovarian cancer is more frequent at older ages, and female longevity has increased.
In comparative terms, ovarian cancers make up about 2-3% of all malignant tumours in women. If we consider only the cases of malignant tumours of the female genital organs, the cases of ovarian cancer are about 18% of them.
Malignant tumours of the ovary can be made up of very different cell types resulting in a diversity of evolution, namely the degree of aggressiveness of the disease. And the same type of tumour, diagnosed and treated at an earlier or later stage of its invasive evolution, may be associated with survivals after 5 years that can range from 15% to 90% (with an average survival of 30-40% after 5 years). In absolute terms, ovarian cancer mortality has remained fairly stable at around 3 per 10,000.
With a much less aggressive evolution compared to other cases of ovarian cancer, there are some rare ovarian tumours called borderline or of low malignant potential, which very rarely progress to full malignancy and, therefore, have a much more favourable prognosis.
Overall, treatments for ovarian cancer include one or more of the following options: surgery, chemotherapy or radiation therapy. It is not within the scope of this text to go into technical details, but it is important to emphasize that there have been advances in the therapeutic area, namely chemotherapy, which bring positive expectations regarding a disease, which, unfortunately, we still do not know how to fully fight.
It is logical to ask questions about whether there are risk factors or whether we can do something that helps to prevent this disease.
As for risk factors, the most important is genetic predisposition, which translates into the family history of cases of the disease. For example, a first-degree relative with the disease is associated with a 3-to-7-fold increase in the risk of ovarian cancer. Some hereditary family syndromes have been identified, in which the risk of ovarian cancer is much higher - breast cancer/ovarian cancer associated with mutations in the BRCA1 and BRCA2 genes, and Lynch syndrome are the most frequent within their rarity.
It is accepted that women who had babies have a 30 to 60% lower risk of ovarian cancer than women without babies. There are some data that point to a greater reduction in risk if the first delivery took place before the age of 30. It is widely discussed, but breastfeeding seems to be a protective factor, with importance directly proportional to its duration. It has been reported that first menstruation very early in life and late menopause may be associated with an increased risk of ovarian cancer, but the evidence is, for the time being, weak. The use of hormone-compensating therapy in the post-menopause period may be associated with a slight increase in risk, especially if its duration is longer than 5 years. However, given the enormous benefits of this therapy and the rarity of ovarian cancer, this slight increase in risk should not prevent the prescription of hormonal therapy women who needs it.
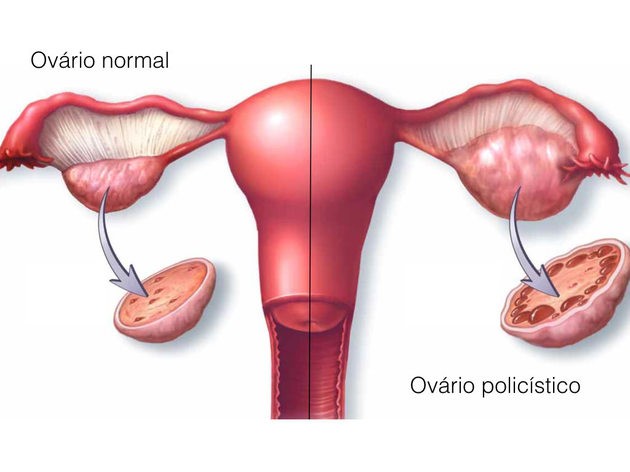
The relationship between some benign gynaecological diseases and ovarian cancer has been much discussed, but there are still no certainties. A long-standing possibility is the increased risk in patients with ovarian endometriosis, a disease that is undoubtedly benign, but which may be associated with an increased risk of some particular types of ovarian cancer. Also, a past of pelvic inflammatory disease appears to correlate with an increased risk of borderline ovarian tumours.
With regard to eating habits and lifestyles, there is no consistent information on a possible relationship between types of food and risk of ovarian cancer. Regular physical exercise seems to be associated with a reduction, albeit small, in the risk of the disease. Smoking is associated with an increased risk for one of the types of invasive ovarian cancer. Apparently, alcohol consumption does not alter the risk of this disease. What is known is that the risk of ovarian cancer is higher in women with a body mass index greater than 30 mg/Km2, that is, obese women.
And what can we do to prevent this disease or to enable an early diagnosis?
Unfortunately, there is no useful methodology for systematic screening. However, the identification of family genetic syndromes may allow surveillance strategies (and possible preventive interventions such as surgery) in these subpopulations. Needless to say, regular health surveillance appointments may contribute to an earlier diagnosis. The enumeration of the main risk factors makes the benefit of avoiding obesity situations obvious, especially after menopause.
In this area, it is established that the use of oral hormonal contraceptives is associated with a significant reduction in the risk of ovarian cancer, with an apparent correlation between the total dose of exposure to the drug and the degree of reduction in the occurrence of ovarian cancer.
In a completely different perspective, with the evolution of medically assisted procreation techniques, there are very encouraging perspectives regarding the chances of preserving the reproductive potential of patients with various types of malignant diseases. Does this apply to patients with ovarian cancer?
Only a small proportion of ovarian cancer cases in patients occur before the age of 40 (9-10% of the total of these tumours, according to the latest published national cancer registry). Theoretically, some of these patients may be candidates for oocyte cryopreservation, with the consequent hope of being able to have a future pregnancy through the use of techniques such as in vitro fertilization. Unfortunately, only a very small fraction of ovarian cancer patients can aspire to resort to oocyte cryopreservation as this type of technique is only feasible at very early stages of the disease (or in borderline tumours) and most ovarian cancers are diagnosed at advanced stages.
Ovarian cancer is an uncommon situation, but of very high severity, even with the most up-to-date treatment methodologies. However, despite the apparent increase in its incidence, mortality has remained stable, which is a positive and encouraging aspect.

Carlos Calhaz Jorge
FMUL Full Professor
Director of the Department of Obstetrics, Gynaecology and Reproductive Medicine at CHULN


